|
Many studies using Finapres Medical Systems have investigated patients' autonomic nervous system function. Our solutions support the clinician in the diagnosis of autonomic failure. Interested? Request for quote |
Autonomic Failure Diagnosis
For over 30 years Finapres Medical Systems have been used by neurologists, cardiologists and researchers to better understand autonomic failure, syncope, POTS, and baroreflex sensitivity (BRS). Many studies using Finapres Medical Systems have been performed to show subjects’ neurological reactions, such as autonomic failure. The Finapres® devices support protocol driven diagnosis of autonomic failure in patients and support documentation of progress due to treatment.
For over 30 years Finapres Medical Systems have been used by neurologists, cardiologists and researchers to better understand autonomic failure, syncope, POTS, and baroreflex sensitivity (BRS). Many studies using Finapres Medical Systems have been performed to show subjects’ neurological reactions, such as autonomic failure. The Finapres® devices support protocol driven diagnosis of autonomic failure in patients and support documentation of progress due to treatment.
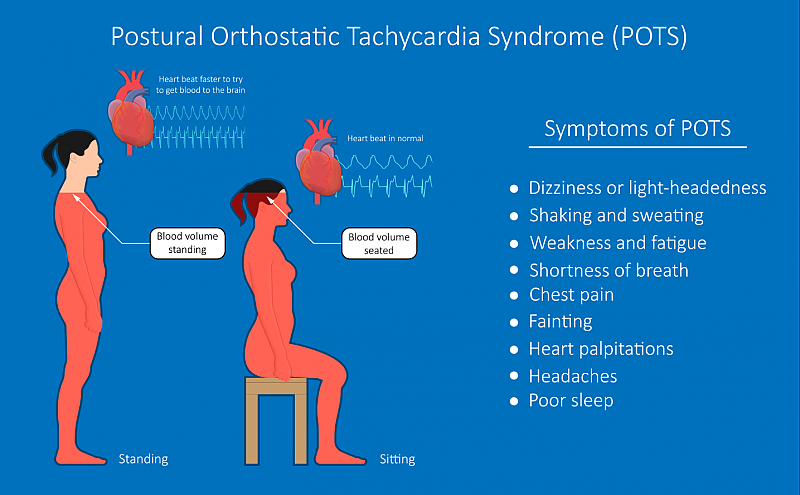
POTS: Postural Orthostatic Tachycardia Syndrome
Postural orthostatic tachycardia syndrome (POTS) is a cardiovascular autonomic disorder characterized by an excessive heart rate increase on standing and orthostatic intolerance, without orthostatic hypotension [1]. About 80% of the POTS patients are female and POTS mainly affects younger individuals (15 to 45 years old). The prevalence of POTS ranges between 0.2% and 1.0% in developed countries. The most common complaints of POTS patients are dizziness, weakness, rapid heartbeat, and palpitation on standing. [2]
Postural orthostatic tachycardia syndrome (POTS) is a cardiovascular autonomic disorder characterized by an excessive heart rate increase on standing and orthostatic intolerance, without orthostatic hypotension [1]. About 80% of the POTS patients are female and POTS mainly affects younger individuals (15 to 45 years old). The prevalence of POTS ranges between 0.2% and 1.0% in developed countries. The most common complaints of POTS patients are dizziness, weakness, rapid heartbeat, and palpitation on standing. [2]
POTS causes and diagnosis
The etiology of POTS is largely unknown. The three main hypotheses include 1: an autoimmune disorder, 2: abnormally increased sympathetic activity and catecholamine excess, and 3: sympathetic denervation leading to central hypovolaemia and reflex tachycardia [2].
Despite its relatively common presentation in the population, POTS, is a relatively misunderstood autonomic disease. Researchers and clinicians struggle to distinguish, diagnose and treat those affected by the condition. A complicating factor is heterogeneity of symptoms that may mask the underlying POTS and divert clinician's attention towards other conditions with a similar presentation [1, 2].
The head-up tilt test and the active stand test are commonly used to diagnose POTS. Both of these autonomic function tests should be performed with non-invasive beat-to-beat hemodynamic monitoring!
The etiology of POTS is largely unknown. The three main hypotheses include 1: an autoimmune disorder, 2: abnormally increased sympathetic activity and catecholamine excess, and 3: sympathetic denervation leading to central hypovolaemia and reflex tachycardia [2].
Despite its relatively common presentation in the population, POTS, is a relatively misunderstood autonomic disease. Researchers and clinicians struggle to distinguish, diagnose and treat those affected by the condition. A complicating factor is heterogeneity of symptoms that may mask the underlying POTS and divert clinician's attention towards other conditions with a similar presentation [1, 2].
The head-up tilt test and the active stand test are commonly used to diagnose POTS. Both of these autonomic function tests should be performed with non-invasive beat-to-beat hemodynamic monitoring!
POTS treatment and quality of life
The most common treatments for POTS include increasing fluid intake, increasing salt, wearing compression stockings, raising the head of the bed (to conserve blood volume), reclined exercises such as rowing, recumbent bicycling and swimming, a healthy diet; avoiding substances and situations that worsen orthostatic symptoms; and finally, the addition of medications meant to improve symptoms [3].
Some patients have mild symptoms and can continue with normal work, school, social and recreational activities. But for others, symptoms may be so severe that normal life activities, such as eating, sitting upright, walking or standing can be significantly limited! Approximately 25% of POTS patients are disabled and unable to work. Researchers found that quality-of-life in POTS patients is comparable to patients on dialysis for kidney failure [3].
The most common treatments for POTS include increasing fluid intake, increasing salt, wearing compression stockings, raising the head of the bed (to conserve blood volume), reclined exercises such as rowing, recumbent bicycling and swimming, a healthy diet; avoiding substances and situations that worsen orthostatic symptoms; and finally, the addition of medications meant to improve symptoms [3].
Some patients have mild symptoms and can continue with normal work, school, social and recreational activities. But for others, symptoms may be so severe that normal life activities, such as eating, sitting upright, walking or standing can be significantly limited! Approximately 25% of POTS patients are disabled and unable to work. Researchers found that quality-of-life in POTS patients is comparable to patients on dialysis for kidney failure [3].
Dizziness: One of the most common symptoms of POTS
References
- Raj, S.R. "The postural tachycardia syndrome (POTS): pathophysiology, diagnosis & management" Indian pacing and electrophysiology journal (2006)
- Fedorowski, A. "Postural orthostatic tachycardia syndrome: clinical presentation, aetiology and management" Journal of internal medicine (2019)
- Dysautonomia international, POTS (2020), http://www.dysautonomiainternational.org/page.php?ID=30
5 relevant facts about syncope
1. Syncope is defined as a transient loss of consciousness (TLOC) due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery. [1]
2. Syncope is a common medical problem, with a frequency between 15% and 39%. In the general population, the annual number episodes are 18-40 per 1000 patients, with similar incidence between genders. [2]
3. The most frequent causes of syncope are [2]
1. Syncope is defined as a transient loss of consciousness (TLOC) due to cerebral hypoperfusion, characterized by a rapid onset, short duration, and spontaneous complete recovery. [1]
2. Syncope is a common medical problem, with a frequency between 15% and 39%. In the general population, the annual number episodes are 18-40 per 1000 patients, with similar incidence between genders. [2]
3. The most frequent causes of syncope are [2]
- the mediated neural reflex, known as neuro-cardiogenic or vasovagal syncope
- heart and blood vessel related issues
- orthostatic hypotension: a drop in blood pressure upon standing
4. Continuous non-invasive blood pressure monitoring, using the Finapres® NOVA, provides various important autonomic tests such as the tilt table test and active stand test.
5. The software packages Autonomic Testing (AT) and Guided Autonomic Testing (GAT) of Finapres support the physician in finding the cause of syncope!
5. The software packages Autonomic Testing (AT) and Guided Autonomic Testing (GAT) of Finapres support the physician in finding the cause of syncope!
References
- Brignole, Michele, et al. “2018 ESC Guidelines for the diagnosis and management of syncope” European Heart Journal 39.21 (2018): 1883-1948
- da Silva, Rose MFL. "Syncope: epidemiology, etiology, and prognosis." Frontiers in physiology 5 (2014): 471.
Find your solutions: